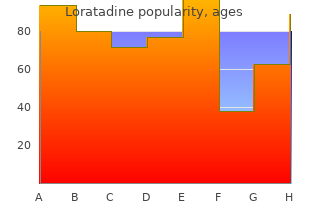
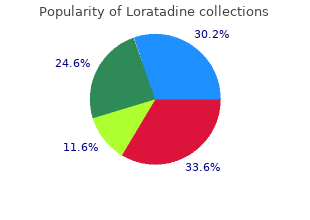
Loratadine
"Buy loratadine 10 mg, allergy medicine for children".
By: E. Boss, M.B. B.CH. B.A.O., M.B.B.Ch., Ph.D.
Co-Director, Boston University School of Medicine
Urgent surgical consultation should be obtained for all patients diagnosed with thoracic aortic dis section regardless of the anatomic location (ascend ing versus descending) as soon as the diagnosis is made or highly suspected allergy testing dayton ohio buy loratadine 10mg on-line. Acute thoracic aortic dissection involving the ascending aorta should be urgently evaluated for emergent surgical repair because of the high risk of associated life-threatening complications such as rupture allergy quiz buy loratadine 10mg. Acute thoracic aortic dissection involving the descending aorta should be managed medically unless life-threatening complications develop (ie allergy forecast fairfax va buy cheap loratadine 10 mg on-line, malperfusion syndrome, progression of dissection, enlarging aneurysm, inability to control blood pressure or symptoms). Recommendation for Surgical Intervention for Acute Thoracic Aortic Dissection Class I 1. For patients with ascending thoracic aortic dissec tion, all aneurysmal aorta and the proximal extent of the dissection should be resected. A partially dissect ed aortic root may be repaired with aortic valve re suspension. Extensive dissection of the aortic root should be treated with aortic root replacement with a composite graft or with a valve sparing root replace ment. It is reasonable to treat intramural hematoma similar to aortic dissection in the corresponding seg ment of the aorta. Recommendation for History and Physical Examination for Thoracic Aortic Disease Class I 1. For patients presenting with a history of acute car diac and noncardiac symptoms associated with a sig nificant likelihood of thoracic aortic disease, the clini cian should perform a focused physical examination, including a careful and complete search for arterial perfusion differentials in both upper and lower ex tremities, evidence of visceral ischemia, focal neuro logic deficits, a murmur of aortic regurgitation, bruits, and findings compatible with possible cardiac tam ponade. Recommendation for Medical Treatment of Patients With Thoracic Aortic Diseases Class I 1. Stringent control of hypertension, lipid profile op timization, smoking cessation, and other atheroscle rosis risk-reduction measures should be instituted for patients with small aneurysms not requiring sur gery, as well as for patients who are not considered surgical or stent graft candidates. Antihypertensive therapy should be administered to hypertensive patients with thoracic aortic diseases to achieve a goal of less than 140/90 mm Hg (pa tients without diabetes) or less than 130/80 mm Hg (patients with diabetes or chronic renal disease) to reduce the risk of stroke, myocardial infarction, heart failure, and cardiovascular death. Beta adrenergic�blocking drugs should be administered to all patients with Marfan syndrome and aortic aneurysm to reduce the rate of aortic dilatation unless contraindicated. For patients with thoracic aortic aneurysm, it is reasonable to reduce blood pressure with beta block ers and angiotensin-converting enzyme inhibitors or angiotensin receptor blockers to the lowest point pa tients can tolerate without adverse effects. An angiotensin receptor blocker (losartan) is reasonable for patients with Marfan syndrome, to reduce the rate of aortic dilatation unless contraindicated. Recommendations for Asymptomatic Patients With Ascending Aortic Aneurysm (see Figures 6 and 7) Class I 1. Asymptomatic patients with degenerative thoracic aneurysm, chronic aortic dissection, intramural he matoma, penetrating atherosclerotic ulcer, mycotic aneurysm, or pseudoaneurysm, who are otherwise suitable candidates and for whom the ascending aorta or aortic sinus diameter is 5. Patients with Marfan syndrome or other genetically mediated disorders (vascular Ehlers Danlos syndrome, Turner syndrome, bicuspid aortic valve, or familial thoracic aortic aneurysm and dissection) should undergo elective operation at smaller diameters (4. Patients undergoing aortic valve repair or replacement and who have an ascending aorta or aortic root of greater than 4. Elective aortic replacement is reasonable for pa tients with Marfan syndrome, other genetic diseases, or bicuspid aortic valves, when the ratio of maximal ascending or aortic root area ( r2) in cm2 divided by the patient�s height in meters exceeds 10. Patients with symptoms suggestive of expansion of a thoracic aneurysm should be evaluated for prompt surgical intervention unless life expectancy from comorbid conditions is limited or quality of life is substantially impaired. Separate valve and ascending aortic replacement are recommended in patients without significant aortic root dilatation, in elderly patients, or in young patients with minimal dilatation who have aortic valve disease. Patients with Marfan, Loeys-Dietz, and Ehlers Danlos syndromes and other patients with dilatation of the aortic root and sinuses of Valsalva should undergo excision of the sinuses in combination with a modified David reimplantation operation if technically feasible or, if not, root replacement with valved graft conduit. For thoracic aortic aneurysms also involving the proximal aortic arch, partial arch replacement to gether with ascending aorta repair using right sub clavian/axillary artery inflow and hypothermic cir culatory arrest is reasonable. Replacement of the entire aortic arch is reasonable for acute dissection when the arch is aneurysmal or there is extensive aortic arch destruction and leakage. Replacement of the entire aortic arch is reasonable for aneurysms of the entire arch, for chronic dissection when the arch is enlarged, and for distal arch aneurysms that also involve the proximal descending thoracic aorta, usually with the elephant trunk procedure. For patients with low operative risk in whom an isolated degenerative or atherosclerotic aneurysm of the aortic arch is present, operative treatment is reasonable for asymptomatic patients when the diameter of the arch exceeds 5. Recommendations for Descending Thoracic Aorta and Thoracoabdominal Aortic Aneurysms Class I 1. For patients with chronic dissection, particularly if associated with a connective tissue disorder, but without significant comorbid disease, and a de scending thoracic aortic diameter exceeding 5.
Preliminary studies point to allergy treatment shot order 10 mg loratadine free shipping certain eating habits in patients with ulcerative colitis that may indicate a potential correlation with disease ac tivity allergy treatment yorba linda ca purchase genuine loratadine line, namely allergy symptoms chest cheap generic loratadine uk, a possibly longer duration of the symptom free interval in patients whose diet contains smaller amounts of sulfur-containing substances. The current state of research, however, does not yet permit a defini tive statement on whether a diet low in sulfur may be beneficial in patients with ulcerative colitis. The currently state of knowledge is inadequate to make a general recommen dation in this regard. Omega-3 fatty acids are found especially in oil derived from ocean fish with naturally high fat content caught in cold waters. Omega-3 fatty acids are known to inhibit the release of substances that promote inflammation. The use of fish oil preparations should not be started without first con sulting your treating physician since no general therapy 32 the informed patient recommendations regarding the use of omega-3 fatty acids have yet been made with regard to their efficacy in patients with inflammatory bowel diseases. Better than using fish oil preparations is the regular (two to three servings per week) consumption of fish, such as salmon, mackerel or herring. A frequent complication in patients with Crohn�s disease is the development of narrowing of the bowel (stenoses). They occur most often near the end of the small bowel (terminal ileum) and frequently necessitate the surgical removal of segments of the small bowel. If the stenosis is an obstacle to the passage of intes tinal contents, a diet low in dietary fiber is often recom mended. This helps prevent the development of certain painful conditions ranging up to obstruction of the bowel. Patients with stenoses should avoid high-fiber foods like asparagus, fennel, green beans and spinach, foods like cabbage, onions and legumes that contribute to bloat ing, as well as hard-skinned fruits. Patients with very significant narrowing may require strained foods or formula diets that do not contain dietary fiber. Inflammation or surgical remov al of this bowel segment, however, has the result that the bile acids reach the colon and are excreted with the stool. The increased excretion of bile acids results in yel low-colored, watery diarrhea (cholegenic diarrhea) with a gradual depletion of the body�s bile acid pool. Bile acids play an important role in the digestion of lipids in that they allow the emulsification of dietary fat in tiny droplets in the small bowel. Persons with a bile acid deficiency experience disturbances of lipid metabolism and fatty stools (steatorrhea). These special fats are sold in health food stores in the form of oil and margarine, and are also used in the preparation of special foods such as pro cessed cheese and hazelnut-nougat desserts. Patients should also use low-fat foods and food preparation methods that do not add large amounts of extra fat. Patients with inflammatory bowel diseases may develop a temporary intolerance of lactose (milk sugar), especial ly during an inflammatory flare. The inflammatory pro cess involves the mucosal membrane of the small bowel resulting in the reduced production of lactase, the en zyme responsible for the digestion of lactose. If a breath test confirms the diagnosis of lactose in tolerance, patients should avoid lactose-containing foods (see table 7) for at least the next three to four weeks. Because most patients tolerate small amounts of lactose, individual testing of tolerance is recommended. Patients with lactose intolerance may still tolerate mod erate amounts of foods such as hard and sliced cheese and sour milk products. This is important for supplying the body�s calcium requirements and reducing the risk of osteoporosis. It is important that lactose-containing foods be taken in small amounts spread out over the whole day. For example, one slice of hard cheese sup plies about a third of the body�s recommended daily al lowance of calcium. On the other hand, there is an in 35 Table 7: Foods containing lactose creasing variety of so-called lactose-free or low-lactose dairy products available in supermarkets. Calcium may also be supplied in the form of high-calcium mineral wa ters (at least 150 mg/liter, > 300 mg/liter is better), calci um-enriched fruit juices, high-calcium vegetables such as broccoli, beets, green cabbage, celery and fennel, as well as soy milk fortified with calcium. Because liquid and tube feeding is more effective and is associated with fewer side effects than parenteral nutri tion (infusion of solutions containing nutrients), they should be preferred to infusions.
Chondrosarcoma mould allergy treatment uk generic loratadine 10 mg otc, the second most common primary malig nant bone tumor allergy treatment vitamin c purchase loratadine toronto, is a large allergy desensitization generic loratadine 10 mg with visa, bulky tumor that may grow and metastasize slowly or very fast, depending upon the charac teristics of the tumor cells involved. Metastatic Bone Disease Metastatic bone disease (secondary bone tumors) is more com mon than any primary malignant bone tumor. The most common primary sites of tumors that metastasize to bone are the kidney, prostate, lung, breast, ovary, and thyroid. Metasta tic tumors most frequently attack the skull, spine, pelvis, femur, and humerus and often involve more than one bone. Clinical Manifestations Bone tumors present with a wide range of associated problems: � Asymptomatic or pain (mild, occasional to constant, severe). This may be accomplished by surgical excision (ranging from local excision to amputation and disarticulation), radiation, or chemotherapy. Nursing Management � Ask the patient about the onset and course of symptoms; assess the patient�s understanding of the disease process, how the patient and the family have been coping, and how the patient has managed the pain. Large bowel obstruction results in an accumulation of intestinal contents, uid, and gas proximal to the obstruction. Obstruction in the colon can lead to severe distention and perforation unless gas and uid can ow back through the ileal valve. If the blood supply is cut off, intestinal strangu lation and necrosis occur; this condition is life threatening. Nursing Management � Monitor symptoms indicating worsening intestinal obstruc tion. The abdominal distention and retention of uid reduce the absorption of uids and stimulate more gastric secretion. With increasing distention, pressure within the intestinal lumen increases, causing a decrease in venous and arteriolar capillary pressure. This causes edema, congestion, necrosis, and eventual rupture or perforation of the intestinal wall, with resultant peritonitis. Vomiting results in loss of hydrogen ions and potassium from the stomach, leading to reduction of chlorides and potassium in the blood and to metabolic alka losis. Clinical Manifestations � Initial symptom is usually crampy pain that is wavelike and colicky. Assessment and Diagnostic Findings Symptoms plus imaging studies (abnormal quantities of gas and/or uid in intestines) and laboratory studies (electrolytes and complete blood count show dehydration and possibly infection) Medical Management Decompression of the bowel may be achieved through a nasogastric or small bowel tube. However, when the bowel is completely obstructed, the possibility of strangulation war rants surgical intervention. Nursing Management � For the nonsurgical patient, maintain the function of the nasogastric tube, assess and measure nasogastric output, assess for uid and electrolyte imbalance, monitor nutri tional status, and assess improvement (eg, return of normal bowel sounds, decreased abdominal distention, subjective improvement in abdominal pain and tenderness, passage of atus or stool). Brain Abscess 99 � Provide postoperative nursing care similar to that for other B abdominal surgeries (see �Preoperative and Postoperative Nursing Management� in Chapter P for additional informa tion). Brain Abscess A brain abscess is a collection of infectious material within the tissue of the brain. An abscess can result from intracranial surgery, pene trating head injury, or tongue piercing. Organisms causing brain abscess may reach the brain by hematologic spread from the lungs, gums, tongue, or heart, or from a wound or intra-abdominal infec tion. It can be a complication in patients whose immune systems have been suppressed through therapy or disease. Prevention To prevent brain abscess, otitis media, mastoiditis, rhinosi nusitis, dental infections, and systemic infections should be treated promptly. Clinical Manifestations � Generally, symptoms result from alterations in intracranial dynamics (edema, brain shift), infection, or the location of the abscess. Medications used include corticosteroids to reduce the in ammatory cerebral edema and antiseizure medications for prophylaxis against seizures (phenytoin, phenobarbital). Nursing Management Nursing interventions support the medical treatment, as do patient teaching activities that address neurosurgical proce dures. Patients and families need to be advised of neurologic de cits that may remain after treatment (hemiparesis, seizures, visual de cits, and cranial nerve palsies). The nurse assesses the family�s ability to express their distress at the patient�s con dition, cope with the patient�s illness and de cits, and obtain support. See �Nursing Management� under associated neuro logic conditions (eg, Epilepsies, Meningitis, or Increased Intracranial Pressure).
Order loratadine online. Eye Allergies.
Diseases
- Symphalangism distal
- Mesodermal defects lower type
- Currarino triad
- Acromesomelic dysplasia Brahimi Bacha type
- Bonnevie Ullrich Turner syndrome
- Hypothermia